Smallpox
Background Information
This Wikipedia selection is available offline from SOS Children for distribution in the developing world. Child sponsorship helps children one by one http://www.sponsor-a-child.org.uk/.
| Smallpox | |
|---|---|
| Classification and external resources | |
 A child infected with smallpox |
|
| ICD- 10 | B 03 |
| ICD- 9 | 050 |
| DiseasesDB | 12219 |
| MedlinePlus | 001356 |
| eMedicine | emerg/885 |
| MeSH | D012899 |
| Variola virus (Smallpox) | |
|---|---|
| Virus classification | |
| Group: | Group I ( dsDNA) |
| Family: | Poxviridae |
| Genus: | Orthopoxvirus |
| Species: | Variola vera |
Smallpox is an infectious disease unique to humans, caused by either of two virus variants named Variola major and Variola minor. The disease is also known by the Latin names Variola or Variola vera, which is a derivative of the Latin varius, meaning spotted, or varus, meaning "pimple". The term "smallpox" was first used in Europe in the 15th century to distinguish variola from the great pox ( syphilis).
Smallpox localizes in small blood vessels of the skin and in the mouth and throat. In the skin, this results in a characteristic maculopapular rash, and later, raised fluid-filled blisters. V. major produces a more serious disease and has an overall mortality rate of 30–35%. V. minor causes a milder form of disease (also known as alastrim, cottonpox, milkpox, whitepox, and Cuban itch) which kills ~1% of its victims. Long-term complications of V. major infection include characteristic scars, commonly on the face, which occurred in 65–85% of survivors. Blindness resulting from corneal ulceration and scarring, and limb deformities due to arthritis and osteomyelitis are less common complications, seen in about 2–5% of cases.
Smallpox is believed to have emerged in human populations about 10,000 BC. The disease killed an estimated 400,000 Europeans each year during the 18th century (including five reigning monarchs), and was responsible for a third of all blindness. Between 20 and 60% of all those infected—and over 80% of infected children—died from the disease.
During the 20th century, it is estimated that smallpox was responsible for 300–500 million deaths. As recently as 1967, the World Health Organization (WHO) estimated that 15 million people contracted the disease and that two million died in that year. After successful vaccination campaigns throughout the 19th and 20th centuries, the WHO certified the eradication of smallpox in 1979. To this day, smallpox is the only human infectious disease to have been completely eradicated.
Cause
Smallpox is caused by infection with variola virus, which belongs to the genus Orthopoxvirus, the family Poxviridae, and subfamily chordopoxvirinae. It affects mostly babies and young children. Variola virus is a large brick-shaped virus measuring approximately 302 to 350 nanometers by 244 to 270 nm, with a single linear double stranded DNA genome consisting of 186 kilobase pairs (kbp) and containing a hairpin loop at each end. The two classic varieties of smallpox are variola major and variola minor. The closest viral relative is molluscum contagiosum, which like smallpox, infects only humans. However, unlike variola species, molluscum infection is benign. The lifecycle of poxviruses is complicated by having multiple infectious forms, with differing mechanisms of cell entry. Poxviruses are unique among DNA viruses in that they replicate in the cytoplasm of the cell rather than in the nucleus. In order to replicate poxviruses produce a variety of specialized proteins not produced by other DNA viruses, the most important of which is a viral-associated DNA-dependent RNA polymerase. Both enveloped and nonenveloped virions are infectious. The viral envelop is made of modified Golgi membranes containing viral-specific polypeptides, including hemagglutinin. Infection with either variola major and variola minor confers immunity against the other.
Four orthopoxviruses cause infection in humans: variola, vaccinia, cowpox, and monkeypox. Variola virus infects only humans in nature, although primates and other animals have been infected in a laboratory setting. Vaccinia, cowpox, and monkeypox viruses can infect both humans and other animals in nature.
Transmission
Transmission of smallpox occurs through inhalation of airborne variola virus, usually droplets expressed from the oral, nasal, or pharyngeal mucosa of an infected person. It is transmitted from one person to another primarily through prolonged face-to-face contact with an infected person, usually within a distance of 6 feet, but can also be spread through direct contact with infected bodily fluids or contaminated objects ( fomites) such as bedding or clothing. Rarely, smallpox has been spread by virus carried in the air in enclosed settings such as buildings, buses, and trains. The virus can cross the placenta, but the incidence of congenital smallpox is relatively low. Smallpox is not notably infectious in the prodromal period and viral shedding is usually delayed until the appearance of the rash, which is often accompanied by lesions in the mouth and pharynx. The virus can be transmitted throughout the course of the illness, but is most frequent during the first week of the rash, when most of the skin lesions are intact. Infectivity wanes in 7 to 10 days when scabs form over the lesions, but the infected person is contagious until the last smallpox scab falls off. Smallpox is highly contagious, but generally spreads more slowly and less widely than some other viral diseases, perhaps because transmission requires close contact and occurs after the onset of the rash. The overall rate of infection is also affected by the short duration of the infectious stage. In temperate areas, the number of smallpox infections were highest during the winter and spring. In tropical areas, seasonal variation was less evident and the disease was present throughout the year. Age distribution of smallpox infections depends on acquired immunity. Vaccination immunity declines over time and is probably lost in all but the most recently vaccinated populations. Smallpox is not known to be transmitted by insects or animals and there is no asymptomatic carrier state.
Signs and symptoms
There are two clinical forms of smallpox. Variola major is the severe and most common form of smallpox, with a more extensive rash and higher fever. There are four types of variola major smallpox based on the Rao classification: ordinary, modified, flat, and hemorrhagic. Historically, variola major has an overall fatality rate of about 30%; however, flat and hemorrhagic smallpox are usually fatal. In addition, a form called variola sine eruptione (smallpox without rash) is seen generally in vaccinated persons. This form is marked by a fever that occurs after the usual incubation period and can be confirmed only by antibody studies or, rarely, by virus isolation.
Variola minor is a less common presentation of smallpox, and a much less severe disease, with historical death rates of 1% or less. Subclinical ( asymptomatic) infections with variola virus have also been noted, but are not believed to be common.
The incubation period between contraction and the first obvious symptoms of the disease is around 12 days. Once inhaled, variola virus invades the oropharyngeal (mouth and throat) or the respiratory mucosa, migrates to regional lymph nodes, and begins to multiply. In the initial growth phase the virus seems to move from cell to cell, but around the 12th day, lysis of many infected cells occurs and the virus is found in the bloodstream in large numbers (this is called viremia), and a second wave of multiplication occurs in the spleen, bone marrow, and lymph nodes. The initial or prodromal symptoms are similar to other viral diseases such as influenza and the common cold: fever (at least 38.5 °C (101 °F)), muscle pain, malaise, headache, prostration, and as the digestive tract is commonly involved, nausea and vomiting and backache often occur. The prodrome, or preeruptive stage, usually lasts 2–4 days. By days 12–15 the first visible lesions—small reddish spots called enanthem—appear on mucous membranes of the mouth, tongue, palate, and throat, and temperature falls to near normal. These lesions rapidly enlarge and rupture, releasing large amounts of virus into the saliva.
Smallpox virus preferentially attacks skin cells, causing the characteristic pimples (called macules) associated with the disease. A rash develops on the skin 24 to 48 hours after lesions on the mucous membranes appear. Typically the macules first appear on the forehead, then rapidly spread to the whole face, proximal portions of extremities, the trunk, and lastly to distal portions of extremities. The process takes no more than 24 to 36 hours, after which no new lesions appear. At this point Variola major infection can take several very different courses.
Ordinary
Ninety percent or more of smallpox cases among unvaccinated persons are of the ordinary type. In this form of the disease, by the second day of the rash, the macules become raised papules. By the third or fourth day the papules fill with an opalescent fluid to become vesicles. This fluid becomes opaque and turbid within 24–48 hours, giving them the appearance of pustules; however, the so-called pustules are filled with tissue debris, not pus.
By the sixth or seventh day, all the skin lesions have become pustules. Between 7 and 10 days the pustules mature and reach their maximum size. The pustules are sharply raised, typically round, tense, and firm to the touch. The pustules are deeply embedded in the dermis, giving them the feel of a small bead in the skin. Fluid slowly leaks from the pustules, and by the end of the second week the pustules deflate, and start to dry up, forming crusts (or scabs). By day 16-20 scabs have formed over all the lesions, which have started to flake off, leaving de-pigmented scars.
Ordinary smallpox generally produces a discrete rash, in which the pustules stand out on the skin separately. The distribution of the rash is densest on the face; more dense on the extremities than on the trunk; and on the extremities, more dense on the distal parts than on the proximal. The palms of the hands and soles of the feet are involved in the majority of cases. In some cases, the blisters merge together into sheets, forming a confluent rash, which begin to detach the outer layers of skin from the underlying flesh. Patients with confluent smallpox often remain ill even after scabs have formed over all the lesions. In one case series, the case-fatality rate in confluent smallpox was 62%.
Modified
Referring to the character of the eruption and the rapidity of its development, modified smallpox occurs mostly in previously vaccinated people. In this form the prodromal illness still occurs but may be less severe than in the ordinary type. There is usually no fever during evolution of the rash. The skin lesions tend to be fewer and evolve more quickly, are more superficial, and may not show the uniform characteristic of more typical smallpox. Modified smallpox is rarely, if ever, fatal. This form of variola major is more easily confused with chickenpox.
Flat
In Flat-type smallpox (also called malignant smallpox) the lesions remain almost flush with the skin at the time when raised vesicles form in ordinary-type smallpox. It is unknown why some people develop this type of disease. Historically, flat-type smallpox accounted for 5%–10% of cases, and the majority (72%) were in children. Flat smallpox is accompanied by a severe prodromal phase that lasts 3–4 days, prolonged high fever, and severe symptoms of toxemia. The rash on the tongue and palate is usually extensive. The skin lesions mature very slowly and by the seventh or eighth day the lesions are flat and appear to be buried in the skin. Unlike ordinary-type smallpox, the vesicles contain very little fluid, are soft and velvety to the touch, and may contain hemorrhages. Flat-type smallpox is nearly always fatal.
Hemorrhagic
Hemorrhagic smallpox is a severe form of smallpox that is accompanied by extensive bleeding into the skin, mucous membranes, and gastrointestinal tract. This form developed in perhaps 2% of infections and occurred mostly in adults. In hemorrhagic smallpox the skin does not blister, but remains smooth. Instead, bleeding occurs under the skin, making the skin look charred and black (this is known as black pox).
In the early, or fulminating, form, hemorrhaging appears on the second or third day as sub- conjunctival bleeding turns the whites of the eyes deep red. Hemorrhagic smallpox also produces a dusky erythema, petechiae, and hemorrhages in the spleen, kidney, serosa, muscle, and, rarely, the epicardium, liver, testes, and bladder. Death often occurs suddenly between the fifth and seventh days of illness, when only a few insignificant skin lesions are present. A later form of the disease occurs in patients who survive for 8–10 days. The hemorrhages appear in the early eruptive period, and the rash is flat and does not progress beyond the vesicular stage. Patients in the early stage of disease show a decrease in platelets, prothrombin, and globulin, and an increase in circulating antithrombin. Patients in the late stage have significant thrombocytopenia; however, deficiency of coagulation factors is less severe. Some in the late stage also show increased antithrombin. This form of smallpox occurs in anywhere from 3–25% of fatal cases (depending on the virulence of the smallpox strain).
Diagnosis
The clinical definition of smallpox is an illness with acute onset of fever greater than 101°F (38.3°C) followed by a rash characterized by firm, deep seated vesicles or pustules in the same stage of development without other apparent cause.
Microscopically, one sees Guarnieri bodies, which are aggregates of the virus. Guarnieri bodies appear as pink blobs. The absence of Guarnieri bodies cannot be used to rule out smallpox, however.
If a clinical case is observed, smallpox is confirmed using laboratory tests. The diagnosis of an orthopoxvirus infection can be made rapidly by electron microscopic examination of pustular fluid or scabs. However, all orthopoxviruses exhibit identical brick-shaped virions by electron microscopy. Definitive laboratory identification of variola virus involves growing the virus on chorioallantoic membrane (part of a chicken embryo) and examining the resulting pock lesions under defined temperature conditions. Strains may be characterized by polymerase chain reaction (PCR) or restriction fragment length polymorphism (RFLP) analysis. Serologic tests and enzyme linked immunosorbent assays (ELISA), which measure variola virus-specific immunoglobulin and antigen have also been developed to assist in the diagnosis of infection.
Chickenpox was commonly confused with smallpox in the immediate post-eradication era. Chickenpox and smallpox can be distinguished by several methods. Unlike smallpox, chickenpox does not usually affect the palms and soles. Additionally, chickenpox pustules are of varying size due to variations in the timing of pustule eruption: smallpox pustules are all very nearly the same size since the viral effect progresses more uniformly. A variety of laboratory methods are available for detecting chickenpox in evaluation of suspected smallpox cases.
Prognosis
The overall case-fatality rate for ordinary-type smallpox is about 30%, but varies by pock distribution: ordinary type-confluent is fatal about 50–75% of the time, ordinary-type semi-confluent about 25–50% of the time, in cases where the rash is discrete the case-fatality rate is less than 10%. The overall fatality rate for children younger than 1 year of age is 40%–50%. Hemorrhagic and flat types have the highest fatality rates. The fatality rate for flat-type is 90% or greater and nearly 100% is observed in cases of hemorrhagic smallpox. The case-fatality rate for variola minor is 1% or less. There is no evidence of chronic or recurrent infection with variola virus.
In fatal cases of ordinary smallpox, death usually occurs between the tenth and sixteenth days of the illness. The cause of death from smallpox is not clear, but the infection is now known to involve multiple organs. Circulating immune complexes, overwhelming viremia, or an uncontrolled immune response may be contributing factors. In early hemorrhagic smallpox, death occurs suddenly about six days after the fever develops. Cause of death in hemorrhagic cases involved heart failure, sometimes accompanied by pulmonary edema. In late hemorrhagic cases, high and sustained viremia, severe platelet loss and poor immune response were often cited as causes of death. In flat smallpox modes of death are similar to those in burns, with loss of fluid, protein and electrolytes beyond the capacity of the body to replace or acquire, and fulminating sepsis.
Complications
Complications of smallpox arise most commonly in the respiratory system and range from simple bronchitis to fatal pneumonia. Respiratory complications tend to develop on about the eighth day of the illness and can be either viral or bacterial in origin. Secondary bacterial infection of the skin is a relatively uncommon complication of smallpox. When this occurs, the fever usually remains elevated.
Other complications include encephalitis (1 in 500 patients), which is more common in adults and may cause temporary disability; permanent pitted scars, most notably on the face; and complications involving the eyes (2% of all cases). Pustules can form on the eyelid, conjunctiva, and cornea, leading to complications such as conjunctivitis, keratitis, corneal ulcer, iritis, iridocyclitis, and optic atrophy. Blindness results in approximately 35% to 40% of eyes affected with keratitis and corneal ulcer. Hemorrhagic smallpox can cause subconjunctival and retinal hemorrhages. In 2% to 5% of young children with smallpox, virions reach the joints and bone, causing osteomyelitis variolosa. Lesions are symmetrical, most common in the elbows, tibia, and fibula, and characteristically cause separation of an epiphysis and marked periosteal reactions. Swollen joints limit movement, and arthritis may lead to limb deformities, ankylosis, malformed bones, flail joints, and stubby fingers.
Treatment
Smallpox vaccination within three days of exposure will prevent or significantly lessen the severity of smallpox symptoms in the vast majority of people. Vaccination four to seven days after exposure likely offers some protection from disease or may modify the severity of disease. Other than vaccination, treatment of smallpox is primarily supportive, such as wound care and infection control, fluid therapy, and possible ventilator assistance. Flat and hemorrhagic types of smallpox are treated with the same therapies used to treat shock, such as fluid resuscitation. Patients with semi-confluent and confluent types of may have therapeutic issues similar to patients with extensive skin burns.
No drug is currently approved for the treatment of smallpox. However, antiviral treatments have improved since the last large smallpox epidemics, and studies suggest that the antiviral drug cidofovir might be useful as a therapeutic agent. The drug must be administered intravenously, however, and may cause serious renal toxicity.
Prevention
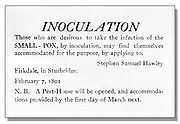
The first attempts to prevent smallpox were practiced in India as early as 1000 BC, and involved either nasal insufflation of powdered smallpox scabs, or scratching material from a smallpox lesion into the skin. This procedure was known as variolation and, if successful, produced lasting immunity to smallpox. However, because the person was infected with variola virus, a severe infection could result, and the person could transmit smallpox to others. Variolation had a 0.5–2% mortality rate; considerably less than the 20–30% mortality rate of the disease itself.
In 1796 Edward Jenner, a doctor in Berkeley, Gloucestershire, rural England, discovered that immunity to smallpox could be produced by inoculating a person with material from a cowpox lesion. Cowpox is a poxvirus in the same family as variola. Jenner called the material used for inoculation vaccine, from the root word vacca, which is Latin for cow. The procedure was much safer than variolation, and did not involve a risk of smallpox transmission. Vaccination to prevent smallpox was soon practiced all over the world. During the 19th century, the cowpox virus used for smallpox vaccination was replaced by vaccinia virus. Vaccinia is in the same family as cowpox and variola but is genetically distinct from both. The origin of vaccinia virus and how it came to be in the vaccine are not known.

The current formulation of smallpox vaccine is a live virus preparation of infectious vaccinia virus. The vaccine is given using a bifurcated (two-pronged) needle that is dipped into the vaccine solution. The needle is used to prick the skin (usually the upper arm) a number of times in a few seconds. If successful, a red and itchy bump develops at the vaccine site in three or four days. In the first week, the bump becomes a large blister (called a “Jennerian vesicle”) which fills with pus, and begins to drain. During the second week, the blister begins to dry up and a scab forms. The scab falls off in the third week, leaving a small scar.
The antibodies induced by vaccinia vaccine are cross-protective for other orthopoxviruses (such as monkeypox, cowpox, and variola (smallpox) viruses). Neutralizing antibodies are detectable 10 days after first-time vaccination, and seven days after revaccination. Historically, the vaccine has been effective in preventing smallpox infection in 95% of those vaccinated. Smallpox vaccination provides a high level of immunity for three to five years and decreasing immunity thereafter. If a person is vaccinated again later, immunity lasts even longer. Studies of smallpox cases in Europe in the 1950s and 1960s demonstrated that the fatality rate among persons vaccinated less than 10 years before exposure was 1.3%; it was 7% among those vaccinated 11 to 20 years prior, and 11% among those vaccinated 20 or more years prior to infection. By contrast, 52% of unvaccinated persons died.
There are side effects and risks associated with the smallpox vaccine. In the past, about 1,000 people for every 1 million people vaccinated for the first time experienced serious, but non-life-threatening, reactions including toxic or allergic reaction at the site of the vaccination ( erythema multiforme), spread of the vaccinia virus to other parts of the body, and to other individuals. Potentially life-threatening reactions occurred in 14 to 52 people out of every 1 million people vaccinated for the first time. Based on past experience, it is estimated that 1 or 2 people in 1 million (0.000198%) who receive the vaccine may die as a result, most often the result of postvaccinial encephalitis or severe necrosis in the area of vaccination (called progressive vaccinia).
Routine childhood smallpox vaccination was discontinued in the United States in 1972. Routine vaccination of healthcare workers was discontinued in 1976, and among military recruits in 1990, though military members deploying to the Middle East have been known to receive it to this day. It is now primarily recommended for laboratory workers at risk for occupational exposure. Mass smallpox vaccination was abandoned in most European countries in the early 1970s.
Eradication
Since Jenner demonstrated the effectiveness of cowpox to protect humans from smallpox in 1796, various attempts were made to eliminate smallpox on a regional scale. As early as 1803, the Spanish Crown organized a mission (the Balmis expedition) to transport the vaccine to the Spanish colonies in the Americas and the Philippines, and establish mass vaccination programs there. In 1842, England banned inoculation, later progressing to mandatory vaccination. The British government introduced compulsory smallpox vaccination by an Act of Parliament in 1853. In the United States, from 1843 to 1855 first Massachusetts, and then other states required smallpox vaccination. Although some disliked these measures, coordinated efforts against smallpox went on, and the disease continued to diminish in the wealthy countries. By 1897, smallpox had largely been eliminated from the United States. In Northern Europe a number of countries had eliminated smallpox by 1900, and by 1914, the incidence in most industrialized countries had decreased to comparatively low levels. Vaccination continued in industrialized countries, until the mid to late 1970s as protection against reintroduction. Australia and New Zealand are two notable exceptions; neither experienced endemic smallpox and never vaccinated widely, relying instead on protection by distance and strict quarantines.
The first hemisphere-wide effort to eradicate smallpox was made in 1950 by the Pan American Health Organization. The campaign was successful in eliminating smallpox from all American countries except Argentina, Brazil, Colombia, and Ecuador. In 1958 Professor Viktor Zhdanov, Deputy Minister of Health for the USSR, called on the World Health Assembly to undertake a global initiative to eradicate smallpox. The proposal (Resolution WHA11.54) was accepted in 1959. At this point, 2 million people were dying every year. Overall, however, progress towards eradication was disappointing, especially in Africa and in the Indian subcontinent. In 1967, the World Health Organization intensified the global smallpox eradication by contributing $2.4 million annually to the effort. An international team, the Smallpox Eradication unit, was formed under the leadership of an American, Donald Henderson.
To eradicate smallpox, each outbreak had to be stopped from spreading, by isolation of cases and vaccination of everyone who lived close by. This process is known as "ring vaccination". The key to this strategy was monitoring of cases in a community (known as surveillance) and containment. The initial problem the WHO team faced was inadequate reporting of smallpox cases, as many cases did not come to the attention of the authorities. The fact that humans are the only reservoir for smallpox infection, and that carriers did not exist, played a significant role to the eradication of smallpox. The WHO established a network of consultants who assisted countries in setting up surveillance and containment activities. Early on donations of vaccine were provided primarily by the Soviet Union and the United States, but by 1973, more than 80% of all vaccine was produced in developing countries.
The last major European outbreak of smallpox was in 1972 in Yugoslavia, after a pilgrim from Kosovo returned from the Middle East, where he had contracted the virus. The epidemic infected 175 people, causing 35 deaths. Authorities declared martial law, enforced quarantine, and undertook massive re-vaccination of the population, enlisting the help of the WHO. In two months, the outbreak was over. Prior to this, there had been a smallpox outbreak in May–July of 1963 in Stockholm, Sweden, brought from the Far East by a Swedish sailor; this had been dealt with by quarantine measures and vaccination of local population.
By the end of 1975, smallpox persisted only in the Horn of Africa. Conditions were very difficult in Ethiopia and Somalia, where there were few roads. Civil war, famine, and refugees made the task even more difficult. An intensive surveillance and containment and vaccination program was undertaken in the spring and summer of 1977. The last naturally occurring case of indigenous smallpox (Variola minor) was diagnosed in Ali Maow Maalin, a hospital cook in Merca, Somalia, on 26 October 1977. The last naturally occurring case of the more deadly Variola major had been detected in October 1975 in a two-year-old Bangladeshi girl, Rahima Banu.
The global eradication of smallpox was certified, based on intense verification activities in countries, by a commission of eminent scientists on 9 December 1979 and subsequently endorsed by the World Health Assembly on 8 May 1980 as Resolution WHA33.3. The first two sentences of the resolution read: "Having considered the development and results of the global program on smallpox eradication initiated by WHO in 1958 and intensified since 1967 … Declares solemnly that the world and its peoples have won freedom from smallpox, which was a most devastating disease sweeping in epidemic form through many countries since earliest time, leaving death, blindness and disfigurement in its wake and which only a decade ago was rampant in Africa, Asia and South America."
Post-eradication
The last cases of smallpox in the world occurred in an outbreak of two cases (one of which was fatal) in Birmingham, England in 1978. A medical photographer, Janet Parker, died from the disease on 11 September 1978, after which the scientist responsible for the unit, Professor Henry Bedson, committed suicide. In light of this accident, all known stocks of smallpox were destroyed or transferred to one of two WHO reference laboratories; the Centers for Disease Control and Prevention (CDC) in the United States and the State Research Centre of Virology and Biotechnology VECTOR in Koltsovo, Russia where a regiment of troops guard it. In 1986, the World Health Organization recommended destruction of the virus, and later set the date of destruction to be 30 December 1993. This was postponed to 30 June 1995. In 2002 the policy of the WHO changed to be against its final destruction. Destroying existing stocks would reduce the risk involved with ongoing smallpox research; the stocks are not needed to respond to a smallpox outbreak. However, the stocks may be useful in developing new vaccines, antiviral drugs, and diagnostic tests.
In March 2004 smallpox scabs were found tucked inside an envelope in a book on Civil War medicine in Santa Fe, New Mexico. The envelope was labeled as containing the scabs and listed the names of the patients they came from. Assuming the contents could be dangerous, the librarian who found them did not open the envelope. The scabs ended up with employees from the CDC who responded quickly once informed of the discovery. The discovery raised concerns that smallpox DNA could be extracted from these and other scabs and used for a biological attack.
Biological warfare
The British may have used smallpox as a biological warfare agent during the French and Indian Wars (1754–63), against France and its Native American allies (see more information at Siege of Fort Pitt). It has been alleged that smallpox was also used as a weapon during the American Revolutionary War (1775–83). During World War II, scientists from the United Kingdom, United States and Japan were involved in research into producing a biological weapon from smallpox. Plans of large scale production were never carried through as they considered that the weapon would not be very effective due to the wide-scale availability of a vaccine. The Soviet Union established a smallpox weapons factory in 1947 in the city of Zagorsk, 75 km to the northeast of Moscow.
An outbreak of weaponized smallpox may have occurred during its testing in the 1970s. General Prof. Peter Burgasov, former Chief Sanitary Physician of the Soviet Army, and a senior researcher within the Soviet program of biological weapons described the incident:
- “On Vozrozhdeniya Island in the Aral Sea, the strongest recipes of smallpox were tested. Suddenly I was informed that there were mysterious cases of mortalities in Aralsk. A research ship of the Aral fleet came 15 km away from the island (it was forbidden to come any closer than 40 km). The lab technician of this ship took samples of plankton twice a day from the top deck. The smallpox formulation—400 gr. of which was exploded on the island—”got her” and she became infected. After returning home to Aralsk, she infected several people including children. All of them died. I suspected the reason for this and called the Chief of General Staff of Ministry of Defense and requested to forbid the stop of the Alma-Ata—Moscow train in Aralsk. As a result, the epidemic around the country was prevented. I called Andropov, who at that time was Chief of KGB, and informed him of the exclusive recipe of smallpox obtained on Vozrazhdenie Island.”
Others contend that the first patient may have contracted the disease while visiting Uyaly or Komsomolsk, two cities where the boat docked.
History
Eurasian epidemics
It is important to note that, although historical epidemics and pandemics are believed by some historians to have been early outbreaks of smallpox, contemporary records are not detailed enough to make a definite diagnosis at this distance.
The Plague of Athens devastated the city of Athens in 430 BC, killing around a third of the population, according to Thucydides. Historians have long considered this an example of bubonic plague, but more recent examination of the reported symptoms led some scholars to believe the cause may have been measles, smallpox, typhus, or a viral hemorrhagic fever (like Ebola).
The Antonine Plague that swept through the Roman Empire and Italy in 165–180 is also thought to be either smallpox or measles. A second major outbreak of disease in the Empire, known as the Plague of Cyprian (251–266), was also either smallpox or measles.
The next major epidemic believed to be smallpox occurred in India. The exact date is unknown. Around 400 AD, an Indian medical book recorded a disease marked by pustules and boils, saying "the pustules are red, yellow, and white and they are accompanied by burning pain … the skin seems studded with grains of rice." The Indian epidemic was thought to be punishment from a god, and the survivors created a goddess, Sitala, as the anthropomorphic personification of the disease. Smallpox was thus regarded as possession by Sitala. In Hinduism the goddess Sitala both causes and cures high fever, rashes, hot flashes and pustules. All of these are symptoms of smallpox.
Smallpox did not definitively enter Western Europe until about 581 when Bishop Gregory of Tours provided an eyewitness account that describes the characteristic findings of smallpox. Most of the details about the epidemic that followed are lost, probably due to the scarcity of surviving written records of early medieval society.
The clearest description of smallpox from pre-modern times was given in the 9th century by the Persian physician, Muhammad ibn Zakarīya Rāzi (Rhazes), who was the first to differentiate smallpox from measles in a treatise on both diseases.
Smallpox was a leading cause of death in the 18th century. It killed an estimated 400,000 Europeans each year in the 18th century, including five reigning European monarchs. Most people became infected during their lifetimes, and about 30% of people infected with smallpox died from the disease.
The Franco-Prussian War triggered a smallpox pandemic of 1870–1875 that claimed 500,000 lives.
Epidemics in the Americas
| Year | Location | Description |
|---|---|---|
| 1520–1527 | Mexico, Central America, South America | Smallpox kills millions of native inhabitants of Mexico. Unintentionally introduced at Veracruz with the arrival of Panfilo de Narvaez on April 23, 1520 and was credited with the victory of Cortes over the Aztec empire at Tenochtitlan (present-day Mexico City) in 1521. Kills the Inca ruler, Huayna Capac, and 200,000 others and destroys the Incan Empire. |
| 1617–1619 | North America northern east coast | Killed 90% of the Massachusetts Bay Indians |
| 1674 | Cherokee Tribe | Death count unknown. Population in 1674 about 50,000. After 1729, 1738, and 1753 smallpox epidemics their population was only 25,000 when they were forced to Oklahoma on the Trail Of Tears. |
| 1692 | Boston, MA | |
| 1702–1703 | St. Lawrence Valley, NY | |
| 1721 | Boston, MA | |
| 1736 | Pennsylvania | |
| 1738 | South Carolina | |
| 1770s | West Coast of North America | Kills out 30% of the West Coast Native Americans |
| 1781–1783 | Great Lakes | |
| 1830s | Alaska | Reduced Dena'ina Athabaskan population in Cook Inlet region of southcentral Alaska by half. Smallpox also devastated Yup'ik Eskimo populations in western Alaska. |
| 1860–1861 | Pennsylvania | |
| 1865–1873 | Philadelphia, PA, New York, Boston, MA and New Orleans, LA | Same period of time, in Washington D.C., Baltimore, MD, Memphis, TN, Cholera and a series of recurring epidemics of Typhus, Scarlet Fever and Yellow Fever |
| 1877 | Los Angeles, CA |
After first contacts with Europeans and Africans, some believe that the death of 90–95% of the native population of the New World was caused by Old World diseases. It is suspected that smallpox was the chief culprit and responsible for killing nearly all of the native inhabitants of the Americas. For more than 200 years, this disease affected all new world populations, mostly without intentional European transmission, from contact in the early 1500s to until possibly as late as the French and Indian Wars (1754–1767).
In 1519 Hernán Cortés landed on the shores of what is now Mexico and was then the Aztec empire. In 1520 another group of Spanish arrived in Mexico from Hispaniola, bringing with them the smallpox which had already been ravaging that island for two years. When Cortés heard about the other group, he went and defeated them. In this contact, one of Cortés's men contracted the disease. When Cortés returned to Tenochtitlan, he brought the disease with him.
Soon, the Aztecs rose up in rebellion against Cortés and his men. Outnumbered, the Spanish were forced to flee. In the fighting, the Spanish soldier carrying smallpox died. After the battle, the Aztecs contracted the virus from the invaders' bodies. Cortes would not return to the capital until August 1521. In the meantime smallpox devastated the Aztec population. It killed most of the Aztec army and 25% of the overall population. A Spanish priest left this description: "As the Indians did not know the remedy of the disease…they died in heaps, like bedbugs. In many places it happened that everyone in a house died and, as it was impossible to bury the great number of dead, they pulled down the houses over them so that their homes become their tombs." On Cortés's return, he found the Aztec army’s chain of command in ruins. The soldiers who lived were still weak from the disease. Cortés then easily defeated the Aztecs and entered Tenochtitlán. The Spaniards said that they could not walk through the streets without stepping on the bodies of smallpox victims.
The effects of smallpox on Tahuantinsuyu (or the Inca empire) were even more devastating. Beginning in Colombia, smallpox spread rapidly before the Spanish invaders first arrived in the empire. The spread was probably aided by the efficient Inca road system. Within months, the disease had killed the Sapa Inca Huayna Capac, his successor, and most of the other leaders. Two of his surviving sons warred for power and, after a bloody and costly war, Atahualpa become the new Sapa Inca. As Atahualpa was returning to the capital Cuzco, Francisco Pizarro arrived and through a series of deceits captured the young leader and his best general. Within a few years smallpox claimed between 60% and 90% of the Inca population, with other waves of European disease weakening them further. A handful of historians argue that a disease called Bartonellosis may have been responsible for some outbreaks of illness, but this opinion is in the scholarly minority. The effects of smallpox were depicted in the ceramics of the Moche people of ancient Peru.
Even after the two mighty empires of the Americas were defeated by the virus and disease, smallpox continued its march of death. In 1633 in Plymouth, Massachusetts, the Native Americans were struck by the virus. As it had done elsewhere, the virus wiped out entire population groups of Native Americans. It reached Mohawks in 1634, the Lake Ontario in 1636, and the lands of the Iroquois by 1679. During the 1770s, smallpox killed at least 30% of the West Coast Native Americans. Smallpox epidemic of 1780–1782 brought devastation and drastic depopulation among the Plains Indians. By 1832, the federal government of the United States established a smallpox vaccination program for Native Americans.
A particularly virulent sequence of smallpox outbreaks took place in Boston, Massachusetts. From 1636 to 1698, Boston endured six epidemics. In 1721, the most severe epidemic occurred. The entire population fled the city, bringing the virus to the rest of the Thirteen Colonies. In the late 1770s, during the American Revolutionary War, smallpox returned once more and killed an estimated 125,000 people. Peter Kalm in his Travels in North America, described how in that period, the dying Indian villages became overrun with wolves feasting on the corpses and weakened survivors.
Famous sufferers and survivors
Famous historical figures who contracted smallpox include Ramesses V, the Kangxi Emperor, Shunzhi Emperor and Tongzhi Emperor of China (official history), Date Masamune of Japan (who lost an eye to the disease), and the Incan emperor Huayna Capac in 1527. More recent public figures also include: Guru Har Krishan 8th Guru of the Sikhs in 1664, Peter III of Russia in 1744. and Maximilian III Joseph, Elector of Bavaria.
Prominent families throughout the world often had several people infected by and/or perish from the disease. For example, several relatives of Henry VIII survived the disease but were scarred by it. These include his sister Margaret, Queen of Scotland, his fourth wife, Anne of Cleves, and his daughter, Elizabeth I of England in 1562 (as an adult she would often try to disguise the pockmarks with heavy makeup). A more distant relative, Mary Queen of Scots, contracted the disease as a child but had no visible scarring.
In Europe, deaths from smallpox often impacted dynastic succession. Louis XV of France succeeded his great-grandfather Louis XIV through a series of deaths of smallpox or measles among those earlier in the succession line. He himself died of the disease in 1774. The only surviving son of Henry VIII, Edward VI, likely died from complications shortly after apparently recovering from the disease, thereby rendering his sire's infamous efforts to provide England with a male heir moot. (His immediate successors were all females.) William III lost his mother to the disease when he was only ten years old in 1660, and named his uncle Charles as legal guardian: her death from smallpox would indirectly spark a chain of events that would eventually lead to the permanent ousting of the Stuart line from the British throne.
Both George Washington and Abraham Lincoln, Presidents of the United States, contracted and recovered from the disease. Joseph Stalin, who was badly scarred by the disease early in life, often had photographs retouched to make his pockmarks less apparent. Crime figure Lucky Luciano contracted disease in 1907 at the age of ten, upon coming to New York from Sicily.
Indian actress Geeta Bali died of small pox in 1965.